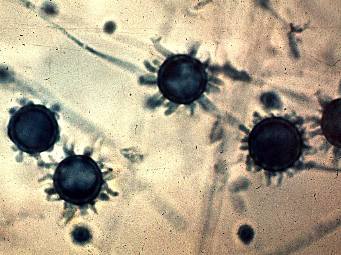
- Babesia microti is the cause of babesiosis in northeastern United States
- intraerythrocytic Babesia destroy the red blood cells causing hemolytic anemia and hemoglobinuria
- mild illness presents with malaise, fatigue, weakness, fever, chills, sweat, headache, myalgia, anorexia, dry cough, arthralgia and nausea
- post-splenectomy, HIV, malignancy and immunosuppression are at risk of severe illness
- symptoms are greater with higher percentage of parasitism
- diagnosed by microscopic examination of Giemsa-stained thin blood smears - round or pear-shaped organism
- asymptomatic need not be treated
- mild illness: oral atovaquone + azithromycin for 7 - 10 days
- severe illness: IV clindamycin + oral quinine for 7 - 10 days