Warfarin reversal: consensus guidelines, on behalf of the Australasian Society of Thrombosis and Haemostasis. MJA 2004


| Agent | Indication |
|---|---|
| Activated charcoal with sorbital | used for many oral toxins |
| Adenosine | Theophylline antidote for adenosine poisoning |
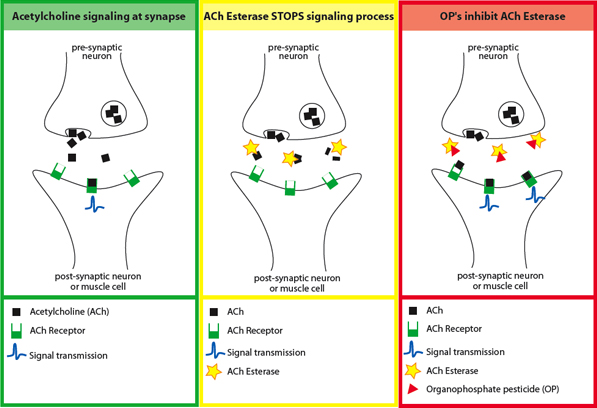
| Atropine | organophosphate and carbamate insecticides,nerve agents, some mushrooms |
| Beta blocker | theophylline |
| Calcium chloride | calcium channel blockers, black widow spider bites |
| Calcium gluconate | hydrofluoric acid |
| Chelators such as EDTA, dimercaprol (BAL), penicillamine, and 2,3-dimercaptosuccinic acid (DMSA, succimer) | heavy metal poisoning |
| Cyanide antidote (amyl nitrite, sodium nitrite, or thiosulfate) | cyanide poisoning |
| Cyproheptadine | serotonin syndrome |
| Deferoxamine mesylate | Iron poisoning |
| Digoxin Immune Fab antibody (Digibind and Digifab) | digoxin poisoning |
| Diphenhydramine hydrochloride and benztropine mesylate | Extrapyramidal reactions associated withantipsychotic |
| Ethanol or fomepizole | ethylene glycol poisoning and methanol poisoning |
| Flumazenil | benzodiazepine poisoning |
| Glucagon | beta blocker poisoning and calcium channel blockerpoisoning |
| 100% oxygen or hyperbaric oxygen therapy (HBOT) | carbon monoxide poisoning and cyanide poisoning |
| Insulin | beta blocker poisoning and calcium channel blockerpoisoning |
| Leucovorin | methotrexate and trimethoprim |
| Methylene blue | treatment of conditions that cause methemoglobinemia |
| Naloxone hydrochloride | opioid poisoning |
| N-acetylcysteine | Paracetamol (acetaminophen) poisoning |
| Octreotide | oral hypoglycemic agents |
| Pralidoxime chloride (2-PAM) | organophosphate insecticides, followed after atropine |
| Protamine sulfate | Heparin poisoning |
| Prussian blue | Thallium poisoning |
| Physostigmine sulfate | anticholinergic poisoning |
| Pyridoxine | Isoniazid poisoning, ethylene glycol |
| Phytomenadione (vitamin K) and fresh frozen plasma | warfarin poisoning and indanedione |
| Sodium bicarbonate | ASA, TCAs with a wide QRS |