- autosomal codominant disorder characterised by elevated plasma levels of LDL-C with normal triglyceride, tendon xanthomas and premature coronary atherosclerosis
- homozygous FH occurs in approximately 1 in 1 million persons worldwide, whereas heterozygous FH occurs in 1 in 500 persons
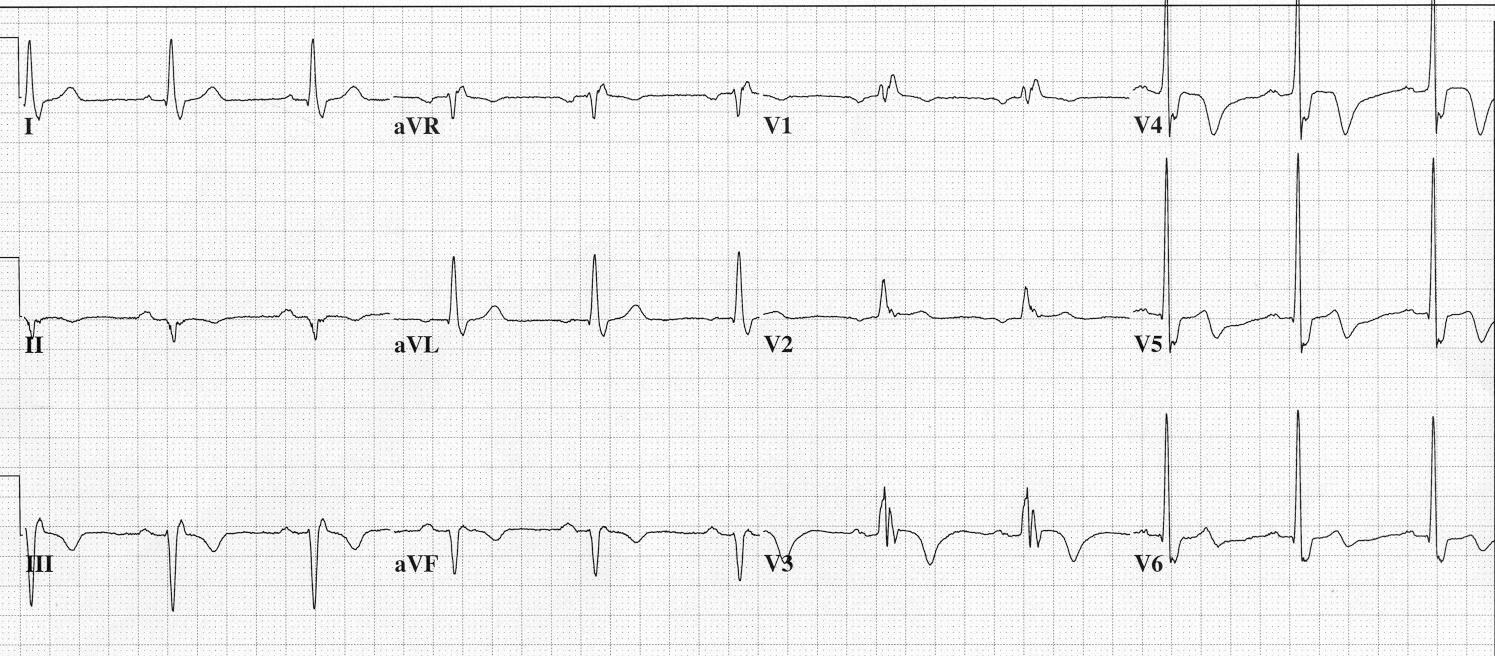
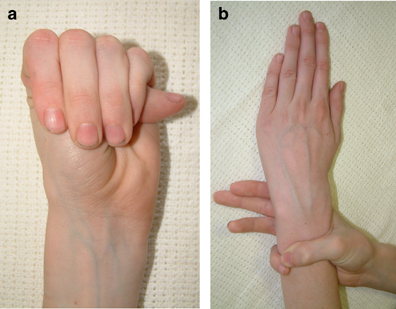
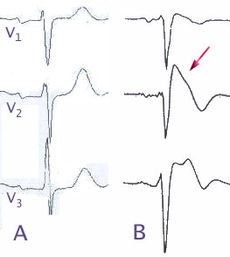
- most homozygous FH present in childhood with cutaneous xanthomas on hand, wrist, elbows, knees, heels, or buttocks. Total cholesterol levels are usually >500mg/dL and devastating complication of homozygous FH is accelerated atherosclerosis
- treatment for FH is LDL apheresis (homozygous) and statin in combination with cholesterol absorption inhibitor
- family history is usually positive for premature atherosclerotic cardiovascular disease