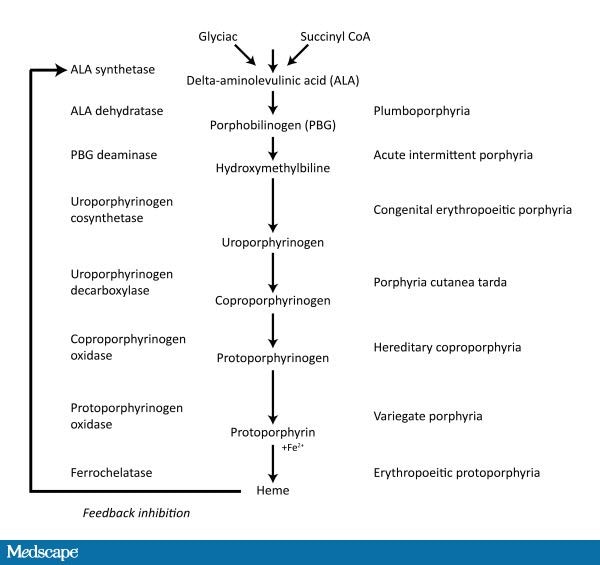
- Porphyrias are group of inherited disease resulting from deficiencies in haem biosynthetic pathway
- Acute porphyrias : acute intermittent porphyria, variegate porphyria, hereditary coproporphyria
- Non acute porphyria : cutaneous hepatic porphyria, congenital porphyria, erythropoeitic protoporphyria
- precipitants of acute attacks are: stress, infection, pregnancy, menstruation, starvation, drugs (sulphonamides, barbiturates, phenytoin)
-
Haematin can help as it acts as negative feedback operator on the porphyrin synthetic pathway
- enzyme inducer exacerbate porphyria as they induce the pathway
- Ehrlich's test: add one volume of Ehrlich reagent to one volume of urine and urine turns red. Add two volumes of chloroform and red colour stays in upper layer
-
Variegate porphyria is associated with
raised urinary & fecal protoporphyrins
- Hereditary coproporphyria is associated with
raised urinary & fecal coproporphyrins
Essential MRCP facts about porphyria
- All porphyrias have
autosomal dominant inheritance
except congenital porphyria
- Only
acute porphyrias develop
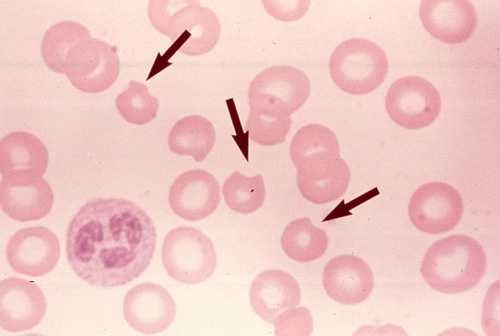
neurological consequence (ALA is neurotoxic)
- All porphyrias are
photosensitive,
except acute intermittent porphyria
- If the name sound's "
inherited" eg.congenital porphyria or hereditary coproporphyria, then it is
extremely rare.
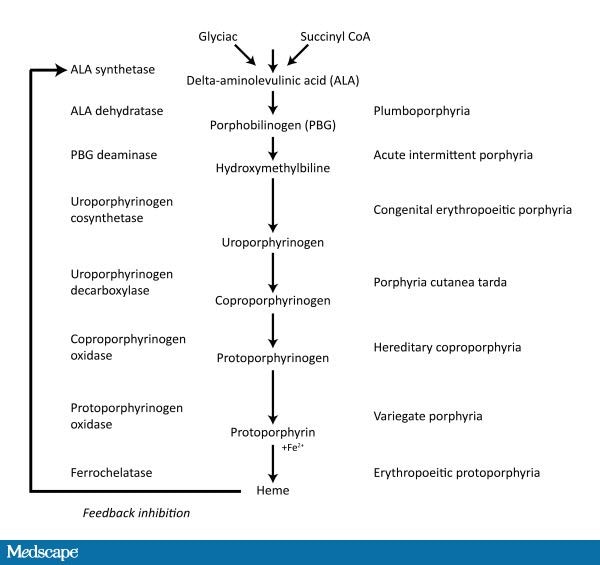
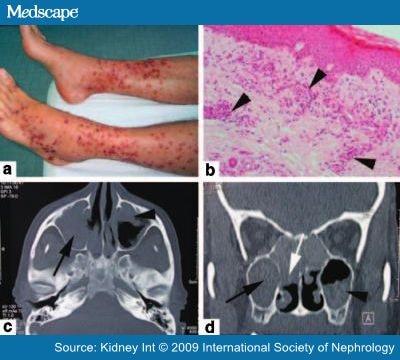
Porphyria cutanea tarda
- most common subtype of porphyria
-
deficient activity of enzyme uroporphyrinogen decarboxylase, causing accumulation of
uroporphyrinogen III
- most common presenting sign is
fragility of sunexposed skin after mechanical trauma, leading to erosion and bullae on dorsal hand, forearm and face
- diagnosis is by
increased plasma and urinary porphyrins
- treatment:
chloroquine, venesection