Polymyositis - reduced amplitude and duration of motor units
Motor neurone disease - fibrillation due to denervation
Myasthenia gravis - diminished response to repetitive stimulation
Lambert Eaton syndrome - enhanced response to repeated stimulation
Myotonia dystrophia - high frequency action potentials (Kamikazee discharge)
Demyelinating neuropathy - slow nerve conduction velocity
Axonal neuropathy - diminished action potential
Total Pageviews
Saturday 31 December 2011
Cluster headache
- a.k.a migrainous neuralgia
- caused by superficial temporal artery smooth muscle hyperperactivity to 5HT
- commoner in male
- rapid onset severe pain around one eye which may become watery and bloodshot with lid swelling, lacrimation, facial flushing, rhinorrhoea, and occasionally transient Horner syndrome
- unilateral, lasts 15-160mins, often nocturnal (waking sufferers at onset of REM sleep)
- treatment: acute attack (100% oxygen at 10-12L/min for 15mins and s/c sumatriptan 6mg or nasal spray sumatriptan 20mg) , prophylaxis (verapamil 120-160mg tds, topiramate)

- caused by superficial temporal artery smooth muscle hyperperactivity to 5HT
- commoner in male
- rapid onset severe pain around one eye which may become watery and bloodshot with lid swelling, lacrimation, facial flushing, rhinorrhoea, and occasionally transient Horner syndrome
- unilateral, lasts 15-160mins, often nocturnal (waking sufferers at onset of REM sleep)
- treatment: acute attack (100% oxygen at 10-12L/min for 15mins and s/c sumatriptan 6mg or nasal spray sumatriptan 20mg) , prophylaxis (verapamil 120-160mg tds, topiramate)

Guillain Barre syndrome
- a.k.a acute autoimmune inflammatory demyelinating polyneuropathy
- segmental demyelination
- 1-2/100,000/year
- bimodal distribution with peak age 15-35 and 50-75 years
- symmetrical ascending muscle weakness preceded by diarrhea (eg:campylobacter) and chest infection (eg: mycoplasma).
- maximal weakness occurs 2 weeks after initial onset of symptom, weakness almost always symmetrical
- other triggers: HIV,EBV, vaccinations, zoster
- associated with autonomic dysfunction (sweating, tachycardia, BP changes, arrhythmias) and hyporeflexia
- monitor force vital capacity (FVC)
- nerve conduction studies: slow conduction
- CSF: albuminocytological dissociation (raised protein, normal cell count)
- GBS is associated with anti-ganglioside GM1 antibody
- Miller-Fisher variant is associated with anti-G1q antibody
- treatment: IVIG, plasmapheresis
- mortality about 10%
- segmental demyelination
- 1-2/100,000/year
- bimodal distribution with peak age 15-35 and 50-75 years
- symmetrical ascending muscle weakness preceded by diarrhea (eg:campylobacter) and chest infection (eg: mycoplasma).
- maximal weakness occurs 2 weeks after initial onset of symptom, weakness almost always symmetrical
- other triggers: HIV,EBV, vaccinations, zoster
- associated with autonomic dysfunction (sweating, tachycardia, BP changes, arrhythmias) and hyporeflexia
- monitor force vital capacity (FVC)
- nerve conduction studies: slow conduction
- CSF: albuminocytological dissociation (raised protein, normal cell count)
- GBS is associated with anti-ganglioside GM1 antibody
- Miller-Fisher variant is associated with anti-G1q antibody
- treatment: IVIG, plasmapheresis
- mortality about 10%
Friday 30 December 2011
Trypanosomiasis
American trypanosomiasis (Chagas' disease)
- caused by T.cruzi
- spread by reduviids (triatomine bugs)
- erythematous indurated nodule (chagoma) at side of infection which may then scar
- fever, myalgia, rash, lymphadenopathy, hepatosplenomegaly, unilateral conjunctivitis, periorbital edema (Romana's sign), myocarditis, meningoencephalitis
- trypomastigotes seen or grown from blood in acute disease, serology in chronic disease
- treatment: nifurtimox, benznidazole


African trypanosomiasis (sleeping sickness)
- T.gambiense (slow, wasting illness), T.rhodesiense (rapidly progressive illness)
- spready by tsetse flies
- tender subcutaneous nodule (chancre) at site of infection
- 2 stages
i) haemolymphatic
- fever, rash, rigors, headache, hepatosplenomegaly, lymphadenopathy
- Winterbottom's sign (posterior cervical node enlargement)
ii) meningoencephalitic
- convulsion, agitation, confusion,apathy, depression, ataxia, dementia, hypersomnolence, coma
- treatment: suramin, melarsoprol


- caused by T.cruzi
- spread by reduviids (triatomine bugs)
- erythematous indurated nodule (chagoma) at side of infection which may then scar
- fever, myalgia, rash, lymphadenopathy, hepatosplenomegaly, unilateral conjunctivitis, periorbital edema (Romana's sign), myocarditis, meningoencephalitis
- trypomastigotes seen or grown from blood in acute disease, serology in chronic disease
- treatment: nifurtimox, benznidazole


African trypanosomiasis (sleeping sickness)
- T.gambiense (slow, wasting illness), T.rhodesiense (rapidly progressive illness)
- spready by tsetse flies
- tender subcutaneous nodule (chancre) at site of infection
- 2 stages
i) haemolymphatic
- fever, rash, rigors, headache, hepatosplenomegaly, lymphadenopathy
- Winterbottom's sign (posterior cervical node enlargement)
ii) meningoencephalitic
- convulsion, agitation, confusion,apathy, depression, ataxia, dementia, hypersomnolence, coma
- treatment: suramin, melarsoprol


Thursday 29 December 2011
Basic statistic (4)
Paired student t test
- compare 2 paired groups of patients with parametric data (normal distribution)
Wilcoxon test
- compare 2 paired groups of patients with non parametric data (skewed distribution)
Unpaired student t test
- compared 2 unpaired groups of patients with parametric data (normal distribution)
Mann-Whitney U test
- compared 2 unpaired groups of patients with non parametric date (skewed distribution)
Chi-squared test
- to compare percentages or proportions of categorical data (2 X 2 contingency table)
- compare 2 paired groups of patients with parametric data (normal distribution)
Wilcoxon test
- compare 2 paired groups of patients with non parametric data (skewed distribution)
Unpaired student t test
- compared 2 unpaired groups of patients with parametric data (normal distribution)
Mann-Whitney U test
- compared 2 unpaired groups of patients with non parametric date (skewed distribution)
Chi-squared test
- to compare percentages or proportions of categorical data (2 X 2 contingency table)
Huntington's disease
- autosomal dominant (full penetrance)
- prevalence: 5:100,000
- a trinucleotide repeat disorder (CAG repeat)
- chromosome 4
- marked loss of neurones in the caudate nucleus and putamen
- increase in protein Huntingtin (polyglutamine)
- dementia, ataxia, abnormal choreiform movements, ophthalmoplegia
- diagnosis by DNA analysis
- treatment: phenothiazine for symptomatic control

- prevalence: 5:100,000
- a trinucleotide repeat disorder (CAG repeat)
- chromosome 4
- marked loss of neurones in the caudate nucleus and putamen
- increase in protein Huntingtin (polyglutamine)
- dementia, ataxia, abnormal choreiform movements, ophthalmoplegia
- diagnosis by DNA analysis
- treatment: phenothiazine for symptomatic control

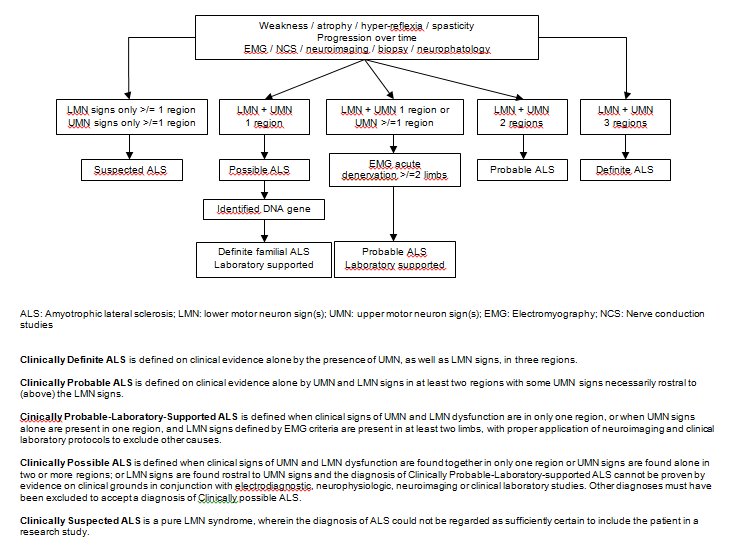
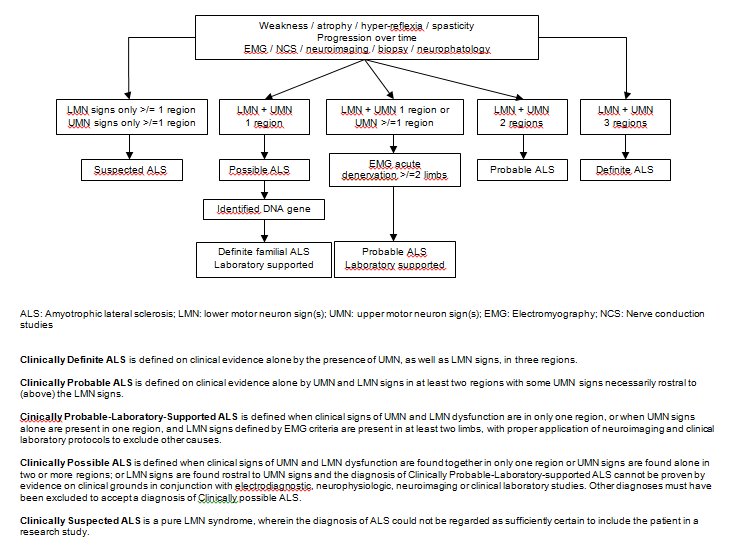
Motor neuron disease
- cluster of major degenerative disease characterised by selective loss of neurons in motor cortex, cranial nerve nuclei, and anterior horn cells
- 4 clinical patterns:
i) amyotrophic lateral sclerosis
ii) progressive bulbar palsy
iii) progressive muscular atrophy - anterior horn cell lesion
iv) primary lateral sclerosis - mainly UMN sign (loss of Betz cell in motor cortex)
- onset more than 50 years of age, with incidence increasing with advancing age
- men affected more frequently
- 5-10% familial (mutation chromosome 21, SOD 1 gene)
- mixed lower motor neuron and upper motor neuron signs
- No sensory loss or sphincter disturbance and never affects eye movement
- 75% presents with limb symptoms, 25% presents with bulbar symptoms (poor prognosis)
- EMG: fasciculation and fibrillation potentials in upper and lower limbs
- El Escorial criteria for ALS (shown below)
- treatment: Riluzole (antiglutamate)
- 4 clinical patterns:
i) amyotrophic lateral sclerosis
ii) progressive bulbar palsy
iii) progressive muscular atrophy - anterior horn cell lesion
iv) primary lateral sclerosis - mainly UMN sign (loss of Betz cell in motor cortex)
- onset more than 50 years of age, with incidence increasing with advancing age
- men affected more frequently
- 5-10% familial (mutation chromosome 21, SOD 1 gene)
- mixed lower motor neuron and upper motor neuron signs
- No sensory loss or sphincter disturbance and never affects eye movement
- 75% presents with limb symptoms, 25% presents with bulbar symptoms (poor prognosis)
- EMG: fasciculation and fibrillation potentials in upper and lower limbs
- El Escorial criteria for ALS (shown below)
- treatment: Riluzole (antiglutamate)
Facioscapulohumeral dystrophy (FSHD)
- autosomal dominant (gene locus 4q35)
- onset 12-14 years old
- initial weakness is seen in facial muscles, starting in orbicularis oculi, orbicularis oris and zygomaticus
- shoulder weakness is common presenting symptom
- signs: weakness of face ('ironed out' expression), winging of scapulae
- life expectancy is normal but up to 15% patients are severely disabled and wheelchair bound

- onset 12-14 years old
- initial weakness is seen in facial muscles, starting in orbicularis oculi, orbicularis oris and zygomaticus
- shoulder weakness is common presenting symptom
- signs: weakness of face ('ironed out' expression), winging of scapulae
- life expectancy is normal but up to 15% patients are severely disabled and wheelchair bound

Foster Kennedy syndrome
- frontal lobe tumor (commonly meningioma in sphenoidal wings)
- causing ipsilateral disc atrophy (compression) + contralateral disc swelling (increased ICP)

- causing ipsilateral disc atrophy (compression) + contralateral disc swelling (increased ICP)

Idiopathic intracranial hypertension
- a.k.a benign intracranial hypertension or pseudotumor cerebri
- most common in obese young women between age 20-50
- headache (worse with straining and bending forward), visual blurring with papilloedema are common features
- 4 diagnostic criteria must be met
i) sign and symptoms of increased ICP
ii) normal or small size ventricles seen on neuroimaging
iii) increased CSF pressure with normal composition
iv) papilledema
- associated factors: OCP, steroids, vitamin A, tetracycline, nitrofurantoin
- opening pressure on LP : >25cm water
- complication: optic nerve infarction or blindness
- treatment: repeated lumbar puncture, acetazolamide, thiazide diuretics, surgical decompression or shunting (lumboperitoneal shunt), trial of steroid for severe cases at risk of visual impairment due to papilloedema, optic nerve fenestration

- most common in obese young women between age 20-50
- headache (worse with straining and bending forward), visual blurring with papilloedema are common features
- 4 diagnostic criteria must be met
i) sign and symptoms of increased ICP
ii) normal or small size ventricles seen on neuroimaging
iii) increased CSF pressure with normal composition
iv) papilledema
- associated factors: OCP, steroids, vitamin A, tetracycline, nitrofurantoin
- opening pressure on LP : >25cm water
- complication: optic nerve infarction or blindness
- treatment: repeated lumbar puncture, acetazolamide, thiazide diuretics, surgical decompression or shunting (lumboperitoneal shunt), trial of steroid for severe cases at risk of visual impairment due to papilloedema, optic nerve fenestration

Angioid streaks
- a.k.a Knapp streaks
- small break in Bruch's membrane
- brown, concentric snake like lines
- Associations
- pseudoxanthoma elasticum
- UGIB
- middle ear deafness
- IHD
- PVD
- floppy mitral valve
- sickle cell disease
- Paget disease
- Ehler Danlos syndrome
- avoid contact sports as it can predispose to globe rupture

- small break in Bruch's membrane
- brown, concentric snake like lines
- Associations
- pseudoxanthoma elasticum
- UGIB
- middle ear deafness
- IHD
- PVD
- floppy mitral valve
- sickle cell disease
- Paget disease
- Ehler Danlos syndrome
- avoid contact sports as it can predispose to globe rupture

Spontaneous bacterial peritonitis
-complication of ascites, diagnosed by ascitic fluid examination which revealed a neutrophil count of > 250 cells/ml
- should be suspected in any ascitic patient who clinically deteriorate, fever and pain can be absent
- abdominal tenderness in more than 50% SBP
- speculated that the infective organism may leak into ascitic fluid via blood or from intestinal overgrowth
- typically caused by aerobic gram negative organism (50% being E.coli)
- treatment : cefotaxime
- should be suspected in any ascitic patient who clinically deteriorate, fever and pain can be absent
- abdominal tenderness in more than 50% SBP
- speculated that the infective organism may leak into ascitic fluid via blood or from intestinal overgrowth
- typically caused by aerobic gram negative organism (50% being E.coli)
- treatment : cefotaxime
Pneumocystis jirovecii (carinii) pneumonia
- one of the AIDS defining illness
- identified on microscopy by methenamine silver staining which shows a cystic phase of organism or Giemsa staining which demonstrates sporozoites and trophozoites with small punctate nuclei
- organism confined to alveolar space with interstitial infiltration of lymphocytes and plasma cells
- presents with high fever, dry cough, exertional dyspnea and type I respiratory failure (arterial oxygen level strikingly lower than expected from symptoms)
- CXR: diffuse bilateral alveolar and interstitial shadowing beginning in perihilar regions and spreading out in a butterfly pattern
- diagnosis can be made in 90% by staining sputum using indirect immunofluorescence with monoclonal antibodies
- prophylaxis/treated with cotrimoxazole (or pentamidine or clindamycin + primaquine if allergic)
- adjunctive steroids have been shown to reduce mortality in severe PCP


- identified on microscopy by methenamine silver staining which shows a cystic phase of organism or Giemsa staining which demonstrates sporozoites and trophozoites with small punctate nuclei
- organism confined to alveolar space with interstitial infiltration of lymphocytes and plasma cells
- presents with high fever, dry cough, exertional dyspnea and type I respiratory failure (arterial oxygen level strikingly lower than expected from symptoms)
- CXR: diffuse bilateral alveolar and interstitial shadowing beginning in perihilar regions and spreading out in a butterfly pattern
- diagnosis can be made in 90% by staining sputum using indirect immunofluorescence with monoclonal antibodies
- prophylaxis/treated with cotrimoxazole (or pentamidine or clindamycin + primaquine if allergic)
- adjunctive steroids have been shown to reduce mortality in severe PCP


Wednesday 28 December 2011
Eczema herpeticum
- a.k.a Kaposi varicelliform eruption
- primary infection of eczematous skin with herpes simplex virus
- may be caused by coxsackievirus A16 or vaccinia virus
- usually an abrupt onset with crops (umbilicated vesicles) appearing over 7-9 days and may become coalesced
- high fever for 7 days
- treatment: acyclovir

- primary infection of eczematous skin with herpes simplex virus
- may be caused by coxsackievirus A16 or vaccinia virus
- usually an abrupt onset with crops (umbilicated vesicles) appearing over 7-9 days and may become coalesced
- high fever for 7 days
- treatment: acyclovir
DNA-containing viruses
- Herpesvirus
- Hepadnavirus
- Adenovirus
- Papovavirus
- Pox virus
- Parvovirus
All DNA viruses are double stranded except Parvovirus

- Hepadnavirus
- Adenovirus
- Papovavirus
- Pox virus
- Parvovirus
All DNA viruses are double stranded except Parvovirus

Ethnic group and genetic disease
Chinese : G6PD deficiency
Northern Europeans : cystic fibrosis
Ashkenazi Jews : Tay Sachs disease, Gaucher disease
Africans : sickle cell disease, thalassemia
Sephardic Jews and Armenians : Familial Mediterranean fever
Scandinavians : AAT, LCAT deficiency
Eskimos : CAH, pseudocholinesterase deficiency
Mediterranean race : thalassemia. G6PD deficency, FMF
Northern Europeans : cystic fibrosis
Ashkenazi Jews : Tay Sachs disease, Gaucher disease
Africans : sickle cell disease, thalassemia
Sephardic Jews and Armenians : Familial Mediterranean fever
Scandinavians : AAT, LCAT deficiency
Eskimos : CAH, pseudocholinesterase deficiency
Mediterranean race : thalassemia. G6PD deficency, FMF
Pseudohypoparathyroidism
- due to mutation of PTH receptor with abnormality of the Gs alpha subunit with reduced cAMP production following a PTH infusion
- hypocalcemia with hyperphosphataemia and elevated PTH
- associated with short stature, low IQ and shortened 4th and 5th metacarpals (Albright's hereditary osteodystrophy)
- pseudopseudohypoparathyroidism is phenotypically similar to pseudohypoparathyroidism but biochemically normal
- both associated with genetic imprinting

- hypocalcemia with hyperphosphataemia and elevated PTH
- associated with short stature, low IQ and shortened 4th and 5th metacarpals (Albright's hereditary osteodystrophy)
- pseudopseudohypoparathyroidism is phenotypically similar to pseudohypoparathyroidism but biochemically normal
- both associated with genetic imprinting

Tuesday 27 December 2011
Familial hypocalciuric hypercalcemia
- autosomal dominant
- mutation in gene on long arm of chromosome 3 encoding for calcium ion sensing G protein coupled receptor in kidney and parathyroid gland
- characterised by lifelong asymptomatic hypercalcemia associated with a relative hypocalciuria and a tendency to hypermagnesemia
- most are misdiagnosed as hyperparathyrodisim, but difference is in FHH, urinary calcium excretion
is low
- commonest presentation is renal stone, and rarely acute pancreatitis
- PTH levels are normal or slightly raised and urinary calcium is low
- can be differentiated from hyperparathyroidism by the calcium creatinine ratio in blood and urine
- mutation in gene on long arm of chromosome 3 encoding for calcium ion sensing G protein coupled receptor in kidney and parathyroid gland
- characterised by lifelong asymptomatic hypercalcemia associated with a relative hypocalciuria and a tendency to hypermagnesemia
- most are misdiagnosed as hyperparathyrodisim, but difference is in FHH, urinary calcium excretion
is low
- commonest presentation is renal stone, and rarely acute pancreatitis
- PTH levels are normal or slightly raised and urinary calcium is low
- can be differentiated from hyperparathyroidism by the calcium creatinine ratio in blood and urine
Monday 26 December 2011
Immunosuppressive for transplantation
Ciclosporin and Tacrolimus
- Both are calcineurin inhibitors, inhibit T cell activation
- ciclosporin forms complexes with cyclophilin whereas tacrolimus binds with immunophilin FK binding protein-12
- both used as rescue agent for treating rejection and as maintenance agent
- levels of both drugs need to be monitored carefully
- both metabolised by cytochrome P450 3A enzyme
- DO NOT cause myelosuppression
Azathioprine
- purine analogue metabolised to mercaptopurine
- prevent cell mediated rejection by blocking purine synthesis
- converted to inactive metabolite by xanthine oxidase (thus, CANNOT give allopurinol!)
- check TPMT (thiopurine methyltransferase) level before initiate treament
- side effects: bone marrow suppression, pancreatitis
Mycophenolate mofetil
- nucleotide inhibitor
- inhibits IMPD (inositol monophosphate dehydrogenase)
- specific for lymphocytes because unlike other cells, an alternative purine synthetic salvage pathway is absent in lymphocytes
- side effects: mostly GI upset, also pancytopenia
Antibodies
- polyclonal : anti-thymocytic globulin (ATG) and anti-lymphocytic globulin (ALG)
- monoclonal : OKT3
- Both are calcineurin inhibitors, inhibit T cell activation
- ciclosporin forms complexes with cyclophilin whereas tacrolimus binds with immunophilin FK binding protein-12
- both used as rescue agent for treating rejection and as maintenance agent
- levels of both drugs need to be monitored carefully
- both metabolised by cytochrome P450 3A enzyme
- DO NOT cause myelosuppression
Azathioprine
- purine analogue metabolised to mercaptopurine
- prevent cell mediated rejection by blocking purine synthesis
- converted to inactive metabolite by xanthine oxidase (thus, CANNOT give allopurinol!)
- check TPMT (thiopurine methyltransferase) level before initiate treament
- side effects: bone marrow suppression, pancreatitis
Mycophenolate mofetil
- nucleotide inhibitor
- inhibits IMPD (inositol monophosphate dehydrogenase)
- specific for lymphocytes because unlike other cells, an alternative purine synthetic salvage pathway is absent in lymphocytes
- side effects: mostly GI upset, also pancytopenia
Antibodies
- polyclonal : anti-thymocytic globulin (ATG) and anti-lymphocytic globulin (ALG)
- monoclonal : OKT3
Membranous glomerulonephritis
- characterised by subepithelial deposits of immune complexes in glomerular basement membrane
- typically seen in the over 40 age group with a male predominance of 2:1
- majority are idiopathic and manifest as nephrotic syndrome
- associations
malignancy (non Hodgkin lymphoma, solid organ tumor)
autoimmune (SLE, RA)
infections (hepatitis B, malaria)
drugs (penicillamine, gold, captopril)
- renal biopsy: thickened GBM and granular IgG and C3 on immunostaining
- 1/3 rapid decline, 1/3 responds to steroids and chlorambucil, 1/3 remit spontaneously
- treatment: low salt diet, fluid restriction, ACE inhibitor, steroids

- typically seen in the over 40 age group with a male predominance of 2:1
- majority are idiopathic and manifest as nephrotic syndrome
- associations
malignancy (non Hodgkin lymphoma, solid organ tumor)
autoimmune (SLE, RA)
infections (hepatitis B, malaria)
drugs (penicillamine, gold, captopril)
- renal biopsy: thickened GBM and granular IgG and C3 on immunostaining
- 1/3 rapid decline, 1/3 responds to steroids and chlorambucil, 1/3 remit spontaneously
- treatment: low salt diet, fluid restriction, ACE inhibitor, steroids
Lupus nephritis
- Overt renal disease occurs in at least one thrid of SLE patients and of these, 25% reach ESRF within 10 years
Classification of lupus nephritis (International Society of Nephrology/Renal Pathological Society 2004)
Class I (Minimal mesangial)
- immune deposits but normal on light microscopy.
- asymptomatic
Class II (Mesangial proliferative)
- mesangial hypercellularity and matrix expansion
- mild renal disease
Class III (Focal)
- involving less than 50% of glomeruli with subdivisions for active or chronic lesions
- presents with hematuria and proteinuria
Class IV (Diffuse)
- involving more than 50% of glomeruli
- classified by the presence of segmental and global lesions as well as active and chronic lesions
- most common and most severe form
- progression to nephrotic syndrome, hypertension and renal insufficiency
Class V (membranous)
- good prognosis
Class VI (advanced sclerosing)
- more than 90% globally sclerosed glomeruli without residual activity
- progressive renal failure
- double stranded DNA levels correlate with lupus nephritis
- drug induced lupus rarely presents with nephritis
Management
- Type 1 requires no treatment
- Type II runs benign course, some require steroids
- Type III, IV, V - steroids and cyclophosphamide / MMF for induction ; azathioprine and MMF for maintenance therapy

Classification of lupus nephritis (International Society of Nephrology/Renal Pathological Society 2004)
Class I (Minimal mesangial)
- immune deposits but normal on light microscopy.
- asymptomatic
Class II (Mesangial proliferative)
- mesangial hypercellularity and matrix expansion
- mild renal disease
Class III (Focal)
- involving less than 50% of glomeruli with subdivisions for active or chronic lesions
- presents with hematuria and proteinuria
Class IV (Diffuse)
- involving more than 50% of glomeruli
- classified by the presence of segmental and global lesions as well as active and chronic lesions
- most common and most severe form
- progression to nephrotic syndrome, hypertension and renal insufficiency
Class V (membranous)
- good prognosis
Class VI (advanced sclerosing)
- more than 90% globally sclerosed glomeruli without residual activity
- progressive renal failure
- double stranded DNA levels correlate with lupus nephritis
- drug induced lupus rarely presents with nephritis
Management
- Type 1 requires no treatment
- Type II runs benign course, some require steroids
- Type III, IV, V - steroids and cyclophosphamide / MMF for induction ; azathioprine and MMF for maintenance therapy

Sunday 25 December 2011
Basic statistic (3)
If a drug reduces the incidence of stroke from 10% to 5%,
Relative risk reduction (RRR) is 50%
Absolute risk reduction (ARR) is 5%
OR
If the absolute risk of stroke is 10%,
the relative risk in treated group is 0.5,
then the absolute risk in treated group is 10 X 0.5 = 5%
the absolute risk reduction is 10% - 5% = 5%
Number needed to treat (NNT) is defined as number needed to treat to prevent 1 death
= 100% / ARR
= 100% / 5%
= 20
Antiphospholipid syndrome
- a.k.a Hughes syndrome
- characterised by recurrent venous/arterial thrombosis and miscarriages
- anticardiolipin antibodies and lupus anticoagulant positive
- paradoxical prolongation of APTT (due to antibody interfering the test), false positive syphilis test
- can cause hypoadrenalism (adrenal vein thrombosis)
- other features: migraine headache, chorea, seizures, transverse myelitis, GBS, livedo reticularis
- aspirin (if wish to get pregnant) or warfarin for patient with thrombotic syndromes

- characterised by recurrent venous/arterial thrombosis and miscarriages
- anticardiolipin antibodies and lupus anticoagulant positive
- paradoxical prolongation of APTT (due to antibody interfering the test), false positive syphilis test
- can cause hypoadrenalism (adrenal vein thrombosis)
- other features: migraine headache, chorea, seizures, transverse myelitis, GBS, livedo reticularis
- aspirin (if wish to get pregnant) or warfarin for patient with thrombotic syndromes

Saturday 24 December 2011
Sickle cell disease
- Hemoglobinopathy caused by substitution of glutamic acid by valine at position 6 (from N terminal) of beta chain
- autosomal recessive
- 2 forms : heterozygous (HbAS) and homozygous (HbSS)
- low partial pressure of oxygen causes HbS to polymerise and precipitate, resulting sickling of erythrocytes.
- HbSS sickle at PO2 of 6kPa and HbAS/HbSC sickle at 4kPa
- Exchange transfusion is indicated when there is neurological damage or visceral sequestration crisis in sickle cell crisis
- most common cause of aplastic crisis is parvovirus infection
- salmonella osteomyelitis is seen in patient with sickle cell anemia
- Sickledex test involves the addition of reagent to blood, turbidity confirms the presence of HbS

- autosomal recessive
- 2 forms : heterozygous (HbAS) and homozygous (HbSS)
- low partial pressure of oxygen causes HbS to polymerise and precipitate, resulting sickling of erythrocytes.
- HbSS sickle at PO2 of 6kPa and HbAS/HbSC sickle at 4kPa
- Exchange transfusion is indicated when there is neurological damage or visceral sequestration crisis in sickle cell crisis
- most common cause of aplastic crisis is parvovirus infection
- salmonella osteomyelitis is seen in patient with sickle cell anemia
- Sickledex test involves the addition of reagent to blood, turbidity confirms the presence of HbS
Target cells and Howell Jolly bodies

- Target cells are red cells with central staining with precipitated haemoglobin seen in conditions with abnormal haemoglobin as well as cell membrane
- Causes are target cells : sickle cell disease, thalassemia, iron deficiency anemia, liver disease
- Howell Jolly bodies contain nuclear remnants
- Causes: post-splenectomy, leukemia, megaloblastic anemia, iron deficiency anemia
Oncogenesis
- Proto-oncogenes found in normal human genomes, have a central role in signal transduction pathway that control cell growth and differentiation
- Mutated proto-oncogenes are called oncogenes (gain of function mutation)
- Examples:
- Ras oncogenes - rhabdomyosarcoma, sporadic tumor (colon and lungs)
- c-myc - Burkitt lymphoma
- N-myc - neuroblastoma
- SRC - sarcoma
- Tumor suppressor gene requires both copies mutation before tumorigenesis occurs. Mutation results in loss of function
- Examples;
- NF-1 - neurofibroma
- BRCA-1 - breast and ovarian cancer
- Rb - retinoblastoma
- VHL - von Hippel Lindau
- p53 - Li Fraumeni syndrome
- Mutated proto-oncogenes are called oncogenes (gain of function mutation)
- Examples:
- Ras oncogenes - rhabdomyosarcoma, sporadic tumor (colon and lungs)
- c-myc - Burkitt lymphoma
- N-myc - neuroblastoma
- SRC - sarcoma
- Tumor suppressor gene requires both copies mutation before tumorigenesis occurs. Mutation results in loss of function
- Examples;
- NF-1 - neurofibroma
- BRCA-1 - breast and ovarian cancer
- Rb - retinoblastoma
- VHL - von Hippel Lindau
- p53 - Li Fraumeni syndrome
Tuesday 20 December 2011
Polycythemia rubra vera
- Primary polycythemia is a clonal stem disorder in which there is excessive proliferation of erythroid, myeloid and megakaryocytic progenitor cells
- over 95% patients with PV have acquired mutations of the gene Janus Kinase 2 (JAK2)
- presents with lethargy, depression, vertigo, itching, gout and visual disturbance
- ruddy cyanosis, plethoric conjunctiva, hypertension, hepatosplenomegaly
- Hb, PCV and RCV are increased
- increased NAP score
- 30% develops myelofibrosis and 5% develop AML
- major complication is bleeding and thrombosis
- treatment: venesection (400-500ml per week, aim PCV < 0.45) or hydroxyurea, H2 receptor antagonist for itchiness, low dose aspirin to prevent thrombosis

- over 95% patients with PV have acquired mutations of the gene Janus Kinase 2 (JAK2)
- presents with lethargy, depression, vertigo, itching, gout and visual disturbance
- ruddy cyanosis, plethoric conjunctiva, hypertension, hepatosplenomegaly
- Hb, PCV and RCV are increased
- increased NAP score
- 30% develops myelofibrosis and 5% develop AML
- major complication is bleeding and thrombosis
- treatment: venesection (400-500ml per week, aim PCV < 0.45) or hydroxyurea, H2 receptor antagonist for itchiness, low dose aspirin to prevent thrombosis

Saturday 17 December 2011
Pacemaker syndrome
- due to AV dyssynchrony
- presents with symptoms of reduced cardiac output (dizziness, syncope, dyspnea, fatigue, weakness, palpitation)
- classically occurs in conjuction with single chamber ventricular pacing
- signs: elevated JVP, cannon A wave, pulmonary edema
- ECG: retrograde P wave
- for ventricularly paced patients, addition of an atrial lead and institution of AV synchronous pacing usually resolves symptoms
- presents with symptoms of reduced cardiac output (dizziness, syncope, dyspnea, fatigue, weakness, palpitation)
- classically occurs in conjuction with single chamber ventricular pacing
- signs: elevated JVP, cannon A wave, pulmonary edema
- ECG: retrograde P wave
- for ventricularly paced patients, addition of an atrial lead and institution of AV synchronous pacing usually resolves symptoms
Cushing's syndrome
- Cushing's syndrome refers to the sustained overproduction of cortisol which causes centripetal obesity with moon face, Buffalo hump, hirsutism, recurrent infection, osteoporosis, hypokalemia, hyperglycemia, proximal myopathy, acne, striae and psychiatric disturbance

- 4 main causes
i) exogenous corticosteroids
ii) Cushing's disease (pituitary adenoma secreting ACTH)
iii) ectopic ACTH production - hypokalemic alkalosis is typical. Caused by small cell lung CA
iv) adrenal adenoma
- In the dexamethasone suppression test, normal individuals suppress cortisol level to less than 50nmol/L
- Incomplete suppression of cortisol following high dose of dexamethasone (2mg QID for 48hours) is typical of Cushing's disease (gold standard is inferior petrosal sinus sampling)
- Metyrapone is an inhibitor of 11 beta hydroxylase, inhibit the conversion of 11 deoxycortisol to cortisol, can be used in treatment of CS

Congenital adrenal hyperplasia
- hirsutism, ambiguous genitalia and precocious puberty in boys
- premature epiphyseal closure is a classical feature
- hyperpigmentation and hyperreninaemia
21-hydroxylase deficiency (commonest)
- raised 17 hydroxyprogesterone is diagnostic
- excess androgen production due to shunting of 17 hydroxyprogesterone into testosterone and androstenedione production
- virilisation may result in clitoromegaly and labial fusion in female at birth
11-beta hydroxylase deficiency (second commonest)
- reduced cortisol leads to increse in ACTH and subsequent increase in production of 11-deoxycorticosterone
- diagnosis made by raised 11-deoxycortisol

Treatment of CAH
- replacement with dexamethasone/hydrocortisone
- efficacy of treatment is monitored by 17OH progesterone or androstenedione levels
- premature epiphyseal closure is a classical feature
- hyperpigmentation and hyperreninaemia
21-hydroxylase deficiency (commonest)
- raised 17 hydroxyprogesterone is diagnostic
- excess androgen production due to shunting of 17 hydroxyprogesterone into testosterone and androstenedione production
- virilisation may result in clitoromegaly and labial fusion in female at birth
11-beta hydroxylase deficiency (second commonest)
- reduced cortisol leads to increse in ACTH and subsequent increase in production of 11-deoxycorticosterone
- diagnosis made by raised 11-deoxycortisol

Treatment of CAH
- replacement with dexamethasone/hydrocortisone
- efficacy of treatment is monitored by 17OH progesterone or androstenedione levels
Clinical drug trials
Phase I
- to establish the human toxicity of a new drug by delivering carefully selected increase doses to fit patients with incurable diseases
Phase II
- to establish the antitumor activity of a drug against a particular tumor in fit patients with incurable diseases
Phase III
- to compare new drug with the best conventional therapy usually by a prospective randomised controlled trials
Phase IV
- to establish the drug efficiency in the adjuvant setting and are use to determine the long term side effects

- to establish the human toxicity of a new drug by delivering carefully selected increase doses to fit patients with incurable diseases
Phase II
- to establish the antitumor activity of a drug against a particular tumor in fit patients with incurable diseases
Phase III
- to compare new drug with the best conventional therapy usually by a prospective randomised controlled trials
Phase IV
- to establish the drug efficiency in the adjuvant setting and are use to determine the long term side effects

Tuesday 13 December 2011
Hemolytic uremic syndrome (HUS)
- characterised by MAHA (microangiopathic hemolytic anemia), thrombocytopenia, and acute kidney injury
- diarrhea associated HUS is associated with E.coli strain O157 (produces verocytotoxin which has A unit which is pathogenic and B unit which facilitate entry of A unit into endothelium)
- non diarrhea HUS is associated with factor H deficiency which is treated with plasmapheresis or plasma infusion
- sporadic cases of HUS is associated with pregnancy, SLE, scleroderma, malignant hypertension, metastatic cancer and HIV
- pneumococcus associated HUS is a rare complication of Strep.pneumoniae infection (antibodies to Thomsen antigen)

- diarrhea associated HUS is associated with E.coli strain O157 (produces verocytotoxin which has A unit which is pathogenic and B unit which facilitate entry of A unit into endothelium)
- non diarrhea HUS is associated with factor H deficiency which is treated with plasmapheresis or plasma infusion
- sporadic cases of HUS is associated with pregnancy, SLE, scleroderma, malignant hypertension, metastatic cancer and HIV
- pneumococcus associated HUS is a rare complication of Strep.pneumoniae infection (antibodies to Thomsen antigen)

Familial mediterranean fever (FMF)
- autosomal recessive
- MEFV gene on chromosome 16 codes for pyrin/marenostrin (activate biosynthesis of chemotactic factor inactivator in neutrophils)
- recurrent attacks of fever, arthritis, serositis, pericarditis, peritonitis
- raised inflammatory markers
- associated with AA amyloidosis causing nephrotic syndrome
- treatment: colchicine

- MEFV gene on chromosome 16 codes for pyrin/marenostrin (activate biosynthesis of chemotactic factor inactivator in neutrophils)
- recurrent attacks of fever, arthritis, serositis, pericarditis, peritonitis
- raised inflammatory markers
- associated with AA amyloidosis causing nephrotic syndrome
- treatment: colchicine
Tuesday 6 December 2011
Pellagra
- triad of Dermatitis, Dementia and Diarrhea
- caused by niacin deficiency
- redness, cracks, chronic thickening, dryness and pigmentation (Casal's necklace or collar)
- painful, red, raw tongue, glossitis and angular stomatitis can occur
- encephalopathy characterised by confusion, disorientation, hallucination and memory loss occur
- neurological manifestation involves CNS and spinal cord where posterior and lateral tracts may be affected
- pellagra may occur in isoniazid therapy, alcohol dependent patients, carcinoid syndrome, Hartnup disease

- caused by niacin deficiency
- redness, cracks, chronic thickening, dryness and pigmentation (Casal's necklace or collar)
- painful, red, raw tongue, glossitis and angular stomatitis can occur
- encephalopathy characterised by confusion, disorientation, hallucination and memory loss occur
- neurological manifestation involves CNS and spinal cord where posterior and lateral tracts may be affected
- pellagra may occur in isoniazid therapy, alcohol dependent patients, carcinoid syndrome, Hartnup disease

Botulism
- paralytic disease caused by neurotoxins of Clostridium botulinum
- due to inhibition of acetylcholine release at neuromuscular junction
- associated with trauma, surgery, subcutaneous heroin injection and sinusitis from intranasal cocaine abuse
- incubation period is 4-14 days
- cranial nerves, bulbar, symmetrical paralysis (diplopia, dysarthria, dry mouth, generalised weakness)
- respiratory failure arises from airway obstruction and diaphragmatic weakness
- diagnosis confirmed by isolation of toxin from serum
- antitoxin is avaiable but risk of anaphylaxis

- due to inhibition of acetylcholine release at neuromuscular junction
- associated with trauma, surgery, subcutaneous heroin injection and sinusitis from intranasal cocaine abuse
- incubation period is 4-14 days
- cranial nerves, bulbar, symmetrical paralysis (diplopia, dysarthria, dry mouth, generalised weakness)
- respiratory failure arises from airway obstruction and diaphragmatic weakness
- diagnosis confirmed by isolation of toxin from serum
- antitoxin is avaiable but risk of anaphylaxis

Monday 5 December 2011
Progressive supranuclear palsy
- early onset of postural instability and vertical gaze palsy (downward)
- often misdiagnosed as Parkinson's disease initially
- unlike PD, tremor is rare, rigidity is worse on neck than limbs
- reduced blinking, which leads to dry eyes and conjunctivitis
- retrocollis and frontalis overactivity leads to startled expression
- akinesia is usually symmetrical from its onset
- often misdiagnosed as Parkinson's disease initially
- unlike PD, tremor is rare, rigidity is worse on neck than limbs
- reduced blinking, which leads to dry eyes and conjunctivitis
- retrocollis and frontalis overactivity leads to startled expression
- akinesia is usually symmetrical from its onset
Sunday 4 December 2011
Mitochondrial myopathies
- mitochondrial diseases are maternally inherited
Chronic progressive external ophthalmoplegia (CPEO)
- slowly progressive paralysis of extraocular muscles
- bilateral, symmetrical, progressive ptosis followed by ophthalmoparesis months to years later
Leber's hereditary optic neuropathy (LHON)
- characterised by blindness, ataxia, peipheral neuropathy and cardiac arrhythmias
- usually affects men, most commonly in the late twenties or early thirties
- commonest cause of blindness in young men
MELAS (myopathy, encephalopathy, lactic acidosis and stroke like episodes)
- lactic acidosis: high lactate to pyruvate ratio
- proximal myopathy, hypotonia, seizure and sttoke like episodes
MERRF (myoclonic epilepsy, ragged red fibres)
- myoclonic seizure that are usually sudden, brief, jerking spasm that can affect the limbs or the entire body
- short stature, deafness, ataxia, dysarthria, optic atrophy, dementia and nystagmus can occur
Kearns-Sayre syndrome
- ophthalmoplegia, heart block, cerebellar ataxia, deafness and mental deficiency
Pearson syndrome
- lactic acidosis, pancreatic insufficiency and pancytopenia

Chronic progressive external ophthalmoplegia (CPEO)
- slowly progressive paralysis of extraocular muscles
- bilateral, symmetrical, progressive ptosis followed by ophthalmoparesis months to years later
Leber's hereditary optic neuropathy (LHON)
- characterised by blindness, ataxia, peipheral neuropathy and cardiac arrhythmias
- usually affects men, most commonly in the late twenties or early thirties
- commonest cause of blindness in young men
MELAS (myopathy, encephalopathy, lactic acidosis and stroke like episodes)
- lactic acidosis: high lactate to pyruvate ratio
- proximal myopathy, hypotonia, seizure and sttoke like episodes
MERRF (myoclonic epilepsy, ragged red fibres)
- myoclonic seizure that are usually sudden, brief, jerking spasm that can affect the limbs or the entire body
- short stature, deafness, ataxia, dysarthria, optic atrophy, dementia and nystagmus can occur
Kearns-Sayre syndrome
- ophthalmoplegia, heart block, cerebellar ataxia, deafness and mental deficiency
Pearson syndrome
- lactic acidosis, pancreatic insufficiency and pancytopenia

Spinal muscular atrophy
- group of disorder characterised by progressive degeneration of the motor neurons of spinal cords and brainstem
- most forms, especially the eariler onset are inherited in an autosomal recessive manner
- 3 common types
Type 1 severe infantile SMA or Werdnig Hoffman disease
Type 2 intermediate type
Type 3 mild juvenile SMA Kugelberg Walander disease
- CK is normal
- EMG: fibrillation secondary to denervation
- muscle biopsy: group atrophy
- most forms, especially the eariler onset are inherited in an autosomal recessive manner
- 3 common types
Type 1 severe infantile SMA or Werdnig Hoffman disease
Type 2 intermediate type
Type 3 mild juvenile SMA Kugelberg Walander disease
- CK is normal
- EMG: fibrillation secondary to denervation
- muscle biopsy: group atrophy
Kennedy's syndrome
- X-linked recessive spinobulbar muscular atrophy
- associated with mutation of androgen receptor gene
- trinucleotide repeat disorder
- perioral fasciculation is a feature
- also presents with cramps, facial weakness, proximal limb weakness, tremor, absent reflexes, fasciculations or dysarthria
- abnormalities are found in androgen receptors leading to gynaecomastia and testicular atrophy
- CK is often elevated

- associated with mutation of androgen receptor gene
- trinucleotide repeat disorder
- perioral fasciculation is a feature
- also presents with cramps, facial weakness, proximal limb weakness, tremor, absent reflexes, fasciculations or dysarthria
- abnormalities are found in androgen receptors leading to gynaecomastia and testicular atrophy
- CK is often elevated

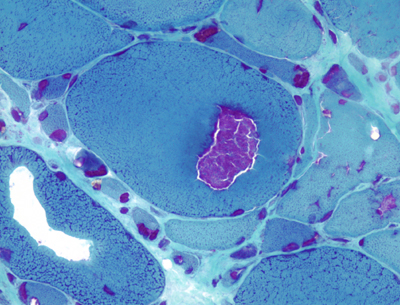
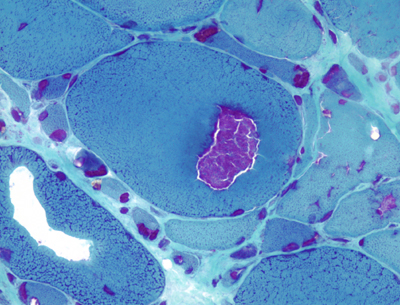
Inclusion body myositis
- idiopathic inflammatory myopathy occur usually in men over 50 years
- gradual muscle weakness (mainly distal)
- weakness finger/wrist flexors out of proportion to finger/wrist extensors and shoulder abductors and weakness of knee extensors disproportionate to the hip flexors (quadriceps and long finger flexors)
- weakness of pharyngeal muscle causes dysphagia in 50%
- mild CK elevation
- muscle biopsy: inflammation and basophilic rimmed vacuoles with diagnostic filamentous inclusions and vacuoles on EM
- IBM is refractory to steroid and immunosuppresive agents
- gradual muscle weakness (mainly distal)
- weakness finger/wrist flexors out of proportion to finger/wrist extensors and shoulder abductors and weakness of knee extensors disproportionate to the hip flexors (quadriceps and long finger flexors)
- weakness of pharyngeal muscle causes dysphagia in 50%
- mild CK elevation
- muscle biopsy: inflammation and basophilic rimmed vacuoles with diagnostic filamentous inclusions and vacuoles on EM
- IBM is refractory to steroid and immunosuppresive agents
Junctional scotoma
- ipsilateral scotoma + contralateral superior quadrantanopia
- lesion at von Willebrand's knee / anterior optic chiasm (eg: meningioma)
- von Willebrand knee is inferonasal fibers of optic nerve which go into the contralateral optic nerve 4mm before crossing over to the opposite optic tract
Friday 2 December 2011
Hepatitis B
- hepatitis B is a hepadnavirus
- HbsAg : first detectable antigen in acute infection but also detectable in chronic infection.
- HbeAg : best marker of infectivity. It denotes viral replications
- anti-HBc (IgM) and HBsAg suggest acute infection. When infection resolves, HBsAg becomes negative and anti-HBc (IgG) is positive
- vaccinated patient : HBsAg is negative and anti-HBs is positive (anti-HBc IgG negative in vaccinated patient but positive in patient recovered from hepatitis B infection)
- most sensitive index of viral replication is HBV DNA
- In pre-core hepatitis B mutant, patient unable to produce HbeAg but high level of viral replication equivalent to eAg positive HBV (highly infectious)
- persistence of HbsAg for more than 6 months defines carrier status and occurs in 5-10% of infections
- HBV DNA and HBeAg levels are measured in response to therapy and undetectable levels would be considered successful treatment
- chronic HBV may respond to PEG interferon alfa-2a or other antivirals
- interferon is indicated for treatment of chronic hepatitis B in e antigen positive patients but is contraindicated for patients with decompensated liver disease
- lamivudine is an inexpensive, safe and effective drug for suppression of hepatitis B virus. Resistance occurs in 15% of patients in 1 year and 60% in 4 years. Adevofir is second line drug for lamivudine resistant hepatitis B virus

- HbsAg : first detectable antigen in acute infection but also detectable in chronic infection.
- HbeAg : best marker of infectivity. It denotes viral replications
- anti-HBc (IgM) and HBsAg suggest acute infection. When infection resolves, HBsAg becomes negative and anti-HBc (IgG) is positive
- vaccinated patient : HBsAg is negative and anti-HBs is positive (anti-HBc IgG negative in vaccinated patient but positive in patient recovered from hepatitis B infection)
- most sensitive index of viral replication is HBV DNA
- In pre-core hepatitis B mutant, patient unable to produce HbeAg but high level of viral replication equivalent to eAg positive HBV (highly infectious)
- persistence of HbsAg for more than 6 months defines carrier status and occurs in 5-10% of infections
- HBV DNA and HBeAg levels are measured in response to therapy and undetectable levels would be considered successful treatment
- chronic HBV may respond to PEG interferon alfa-2a or other antivirals
- interferon is indicated for treatment of chronic hepatitis B in e antigen positive patients but is contraindicated for patients with decompensated liver disease
- lamivudine is an inexpensive, safe and effective drug for suppression of hepatitis B virus. Resistance occurs in 15% of patients in 1 year and 60% in 4 years. Adevofir is second line drug for lamivudine resistant hepatitis B virus

Thursday 1 December 2011
Horner's syndrome
- unilateral pupillary constriction with slight ptosis and enophthalmos indicates a sympathetic pathway lesion on ipsilateral side
- diminution of sweating on the same side depends upon the level of lesion
i) central lesion : entire half of head, arm and upper trunk
ii) neck lesion proximal to superior cervical ganglion (preganglionic): diminished facial sweating
iii) lesion distal to superior cervical ganglion (postganglionic) : do not affect sweating at all
- Iris heterochromia if congenital or long standing
- Tests
i) 4% cocaine drop (Horner does not dilate)
ii) 1% hydroxyamphetamine (post ganglionic Horner does not dilate)

- diminution of sweating on the same side depends upon the level of lesion
i) central lesion : entire half of head, arm and upper trunk
ii) neck lesion proximal to superior cervical ganglion (preganglionic): diminished facial sweating
iii) lesion distal to superior cervical ganglion (postganglionic) : do not affect sweating at all
- Iris heterochromia if congenital or long standing
- Tests
i) 4% cocaine drop (Horner does not dilate)
ii) 1% hydroxyamphetamine (post ganglionic Horner does not dilate)

Atrial septal defect
- accounts for 10-15% of all congenital cardiac anomalies
- more common in women than men (2:1)
- 2 types: ostium secundum (75%) and ostium primum
- complications rarely occur in childhood, but prolonged shunting leads to pulmonary hypertension, atrial fibrillation, Eisenmenger syndrome, but not risk of endocarditis
- sign: pulmonary flow murmur, splitting of second heart sound
- ECG: RBBB & RAD (secundum) ; RBBB & LAD (primum)
- association: Holt Oram syndrome (ASD with triphalangeal thumb and radial abnormalities); Lutembacher syndrome (ASD and MS)
- treatment: ASD closure before age of 10 years old
- Uncorrected, 70% develop symptoms by age of 40

- more common in women than men (2:1)
- 2 types: ostium secundum (75%) and ostium primum
- complications rarely occur in childhood, but prolonged shunting leads to pulmonary hypertension, atrial fibrillation, Eisenmenger syndrome, but not risk of endocarditis
- sign: pulmonary flow murmur, splitting of second heart sound
- ECG: RBBB & RAD (secundum) ; RBBB & LAD (primum)
- association: Holt Oram syndrome (ASD with triphalangeal thumb and radial abnormalities); Lutembacher syndrome (ASD and MS)
- treatment: ASD closure before age of 10 years old
- Uncorrected, 70% develop symptoms by age of 40

Subscribe to:
Posts (Atom)